Many benefits leaders are tasked with managing a complex portfolio of point solutions—ranging from virtual physical therapy to specialty care—all intended to enrich benefit packages, improve health outcomes and reduce overall spend. The core challenge often lies in discerning which solutions are genuinely delivering a true ROI. Vendors promise transformative savings, but if all those projections held true, your benefits program would be making you money.
Specialty care—including surgery—accounts for a significant 50% of employer healthcare spend, and its growth is outpacing other areas. Because of this, it’s critical to achieve a clear, accurate understanding of these costs and the actual savings your solutions deliver.
In this webinar, you’ll hear from:
- Denise King, VP, Global Benefits and Payroll, Medtronic
- Candace Jodice, Employer Benefits Executive & Digital Health/Wellbeing Solutions Advisor
- Erin Tatar, Senior VP, Consultant Relations, Lantern (Host)
Key Takeaways:
- How to set an accurate baseline to understand savings
- What to look for in a specialty care solution that delivers hard-dollar savings
- Tips to ensure you’re not sacrificing quality care for cost reductions
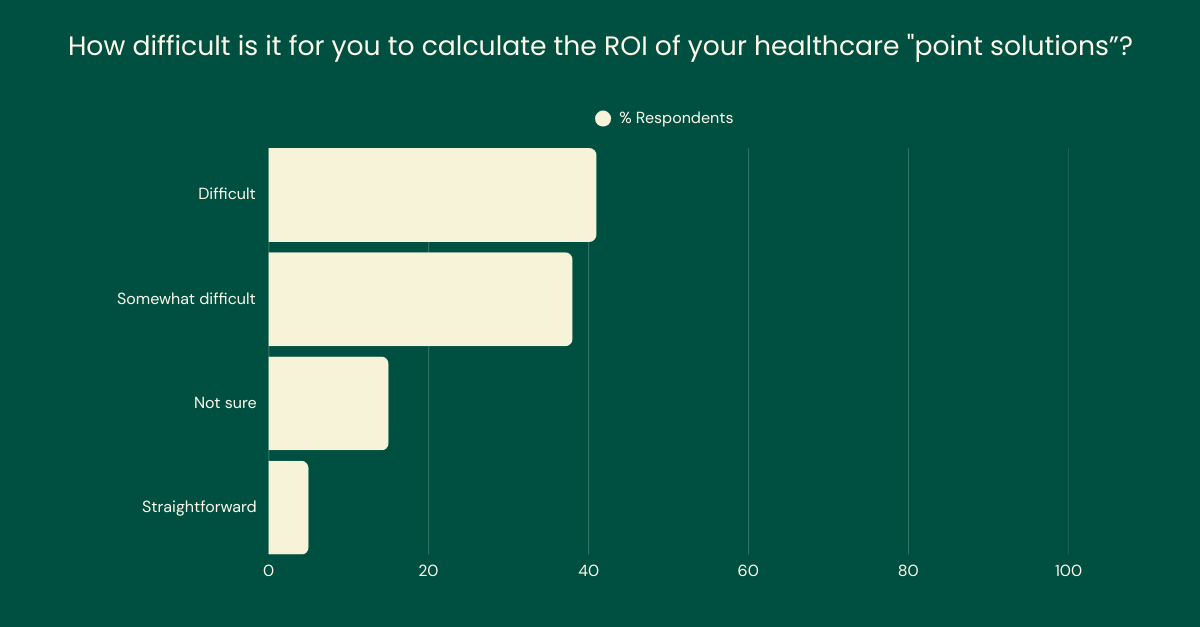
The Difficulty in Calculating Healthcare Benefits ROI
A poll conducted with benefits leaders during the webinar confirmed a widespread sentiment: calculating ROI for healthcare programs is overwhelmingly “difficult” or “somewhat difficult.”
“I tell every point solution when they present their ROI calculation to me that that is just smoke and mirrors,” said Denise King, VP of Global Benefits and Payroll at Medtronic. “There is no vendor that will ever admit that their solution didn’t save me any money. And if I had all of the savings that these vendors have claimed to provide over the years, I’d actually be generating revenue for the company.”
Part of this complexity lies in the reliance on “soft-dollar” savings—those indirect, less immediately quantifiable benefits such as improved productivity or employee satisfaction. While these are important considerations, they often involve predicting and quantifying “what didn’t happen.”
“Soft dollar savings are important, but they’re usually not the key focus, especially when you’re trying to sell a program to your CFO,” said Candace Jodice, an independent advisor and former benefits leader at CVS Health. However, she also recognized their value in addressing “employee noise” and enhancing the healthcare experience.
Setting an Accurate Baseline
Before any savings can be meaningfully calculated, organizations need a transparent understanding of their current spending—a task often complicated by the inherent messiness of healthcare data.
“Surgical care alone makes up 20 to 25% of that spend, but most of us don’t have a great handle on that,” explained Erin Tatar, Senior VP at Lantern.
She pointed out that typical reporting often obscures this specific spend, and significant variation exists in both the cost and quality within surgical care. Common data flaws—such as deleted anesthesia codes, omitted implant costs, or incorrect site-of-care codes—can significantly distort the perception of current costs.
King shared Medtronic’s own experience in this area: “It is difficult… because as you’ve said already, the cost is embedded in our top spend category, so we can look at cancer and MSK, but it’s trickier to really understand what those avoidable surgical costs are.”
Further challenges include inconsistent data from multiple partners, varying claim lags, and differing definitions of episodes of care, Jodice added. She said attributing savings to a single program also becomes difficult when multiple initiatives may be influencing overall spend.
I remember saying early on in one of my evaluations, ‘Obviously we want to pay you for what you do, but you have to be honest, you have to be transparent, or we’re going to just move on and talk to somebody else.’
Unpacking Vendor Savings Calculations
Once a baseline is established, the next hurdle is to clearly understand how vendors are calculating their projected savings.
“My question really is always around what are they doing to work with their customers to really develop a meaningful ROI calculation that actually tells me a story that I can trust,” King says. She advocates for vendors to collaborate with their clients to define how ROI should be calculated, moving away from proprietary, often opaque methodologies.
Jodice emphasized the foundational need for transparency and trust, especially when benefits leaders are relying on projected savings to manage overall costs. “I remember saying early on in one of my evaluations, ‘Obviously we want to pay you for what you do, but you have to be honest, you have to be transparent, or we’re going to just move on and talk to somebody else,’” she shared, adding that when vendors are willing to place their fees at risk, they’re suddenly really cautions about how they’re actually calculating the savings.
In response to this pervasive industry challenge, Lantern has taken the initiative of publishing its TrueRate Savings Methodology, inviting industry-wide feedback and collaboration.
“What stood out was the willingness to, number one, take this on and recognize that you need to do better for employers… and then taking that feedback to really go out and build something—that is a very, very good start,” King said.
Ensure High-Quality Care to Increase Engagement and See More Savings
The ultimate objective extends beyond cost reduction to encompass high-quality care that fosters better health outcomes. “I want to see that that total cost of care is lower. I want to see fewer complications,” King stated, noting that Medtronic also plans to analyze metrics like shorter disability durations over time.
Lantern, for instance, vets its network at the individual surgeon level, considering factors like board certification, fellowship training, procedure volumes and appropriateness of care. King underscored the importance of this physician-level assessment, rather than relying solely on a facility’s reputation.
While standard clinical measures like complication and readmission rates are “table stakes,” Jodice said the overall employee experience can significantly influence a program’s success. “People will associate high-value care with what they experience in the system.” she said.
Happy employees, getting the best care is important to Medtronic. “What we hear from employees about Lantern has been overwhelmingly positive, which is a nice change,” King said.
Navigating the Future of Specialty Care
The journey toward accurate ROI and impactful specialty care programs is evolving. Benefits leaders generally allow new point solutions about two to three years to demonstrate meaningful results before considering alternatives, underscoring the importance of setting clear expectations and performance metrics from the outset.
To effectively manage specialty care spend, benefits leaders must have a steadfast commitment to data accuracy, a persistent call for vendor transparency, and an unwavering focus on both quality outcomes and the member experience.
By asking insightful questions, fostering collaborative vendor partnerships and advocating for more standardized methodologies, benefits leaders can navigate away from ambiguity and guide their organizations toward sustainable, high-value healthcare that truly serves their employees.
Get a clear picture of your healthcare spend
Download Lantern’s TrueRate Savings Methodology